Introduction :
Primary central nervous system lymphoma (PCNSL) is a rare diffuse large B-cell lymphoma (DLBCL) with distinct clinical and biological features, characterized by an aggressive course and poor prognosis. Patients with relapsed/refractory (R/R) disease have an unmet medical need due to a median overall survival (OS) of only 6.8 months. Novel therapies are urgently required for patients with R/R CNSL. In June 2020, the U.S. Food and Drug Administration granted accelerated approval to selinexor for the treatment of adult patients with R/R DLBCL. Selinexor has demonstrated central nervous system (CNS) penetration and activity in secondary CNS lymphoma (SCNSL) patients. Thus, we conducted a retrospective review of PCNSL/SCNSL cases treated with a selinexor-based regimen to preliminarily evaluate its effectiveness and safety.
Methods:
We retrospectively analyzed the medical records of 13 patients with CNSL who received selinexor-based combination therapy between June 2021 and June 2023 at three research centers in China. Among these cases, 2 were previously untreated, and 11 were relapsed or refractory patients. All patients had histopathologically confirmed DLBCL at the time of initial diagnosis. Data collection included baseline characteristics, treatment efficacy and safety evaluation.
Results:
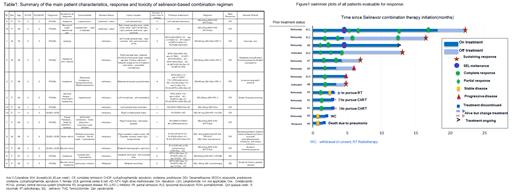
A total of 13 patients (10 PCNSL and 3 SCNSL) were included in the study, with a median age of 62 years (range, 28-73), including three male patients. The median international extranodal lymphoma study group (IELSG) score for PCNSL cases was 3 (range, 1-3). The median International Prognosis Index (IPI) score for the three systemic DLBCL cases was 5 (range, 3-5), and three cases were at Ann Arbor stage IV. Among the patients, 11 had relapsed or refractory disease with a median of 2 prior treatments (range, 1-4), and 10 of them were refractory to previous treatments. The main patient characteristics, responses, and toxicities of the selinexor-based combination regimen are summarized in Table 1.
Figure 1 presents the response of all evaluable patients. The overall response rate (ORR) of the patients was 84.6% (11 /13), with a complete response (CR) rate of 76.9% (10/13). Both treatment-naïve patients achieved CR after four and six cycles of the selinexor-containing first-line regimen, respectively. They are currently experiencing sustained remission, with the longest duration reaching 13 months. For relapsed/refractory CNSL, the ORR and CR rate were 81.8% (9/11) and 72.7% (8/11), respectively. Two patients had stable disease (SD). Among the 9 patients who achieved remission, 4 patients are still in remission, with the longest duration reaching 20 months, 2 patients received CART bridging therapy, one received radiation therapy, and 2 patients experienced disease progression after 5 months, but all are currently still alive. These patients are currently under continuous observation.
Due to the heterogeneity of the selinexor-based regimens, the categories and severity of adverse events (AEs) varied greatly among the different regimens. The median treatment cycle number was six (range, 2-22). One patient died due to pneumonia infection, one patient was lost to follow-up, three patients successfully bridged to CART/RT, and eight patients completed the treatment as planned. The common AEs included thrombocytopenia, infection, nausea, vomiting, and gastrointestinal bleeding(Table 1).
Conclusion:
This report provides encouraging evidence of the efficacy and tolerable safety of the selinexor-based regimen in the treatment of CNSL. However, further prospective studies with a larger sample size are needed to provide more comprehensive evidence regarding the efficacy of selinexor in central nervous system lymphoma and to determine the appropriate dosage and optimal combination strategies.v
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal